What Do I Need to Know about Lung Cancer Screening?
More in this issueLAU interventional pulmonologist outlines the benefits and risks of lung cancer screening.
Lung cancer is the most common cancer in men, the third most common cancer in women, and the leading cause of cancer deaths worldwide. In 2018, there were two million new cases of lung cancer worldwide, accounting for 1.8 million deaths in the same year.
Lebanon has the second highest incidence of lung cancer in males and the highest incidence of lung cancer in females in the Middle East and North Africa (MENA) region. Lung cancer is the third most common cancer in Lebanon after breast and bladder cancer, and its incidence in the country is on the rise. It accounts for 9.2 percent of all newly diagnosed cancer cases in Lebanon with 1,641 new cases diagnosed in 2018. It is also the most common cause of cancer deaths in the country accounting for 1,490 deaths or 16.6 percent of cancer deaths.
The lung cancer five-year survival rate (18.6 percent) is lower than many other common cancers, such as colorectal (64.5 percent), breast (89.6 percent) and prostate (98.2 percent). The five-year survival rate for lung cancer is 56 percent for cases detected when the disease is still localized (within the lungs). However, only 16 percent of lung cancer cases are diagnosed at an early stage. For distant tumors (spread to other organs) the five-year survival rate is only 5 percent. More than half of people with lung cancer die within one year of being diagnosed.
Lung cancer typically presents with chest pain, a cough, shortness of breath, or coughing up of blood. But, by the time the symptoms occur, the cancer is usually at a more advanced stage. Therefore, it is crucial that it is diagnosed before the symptoms set in. This can be done through screening, which can detect early stage lung cancer so that it may be treated with surgery or other modalities.
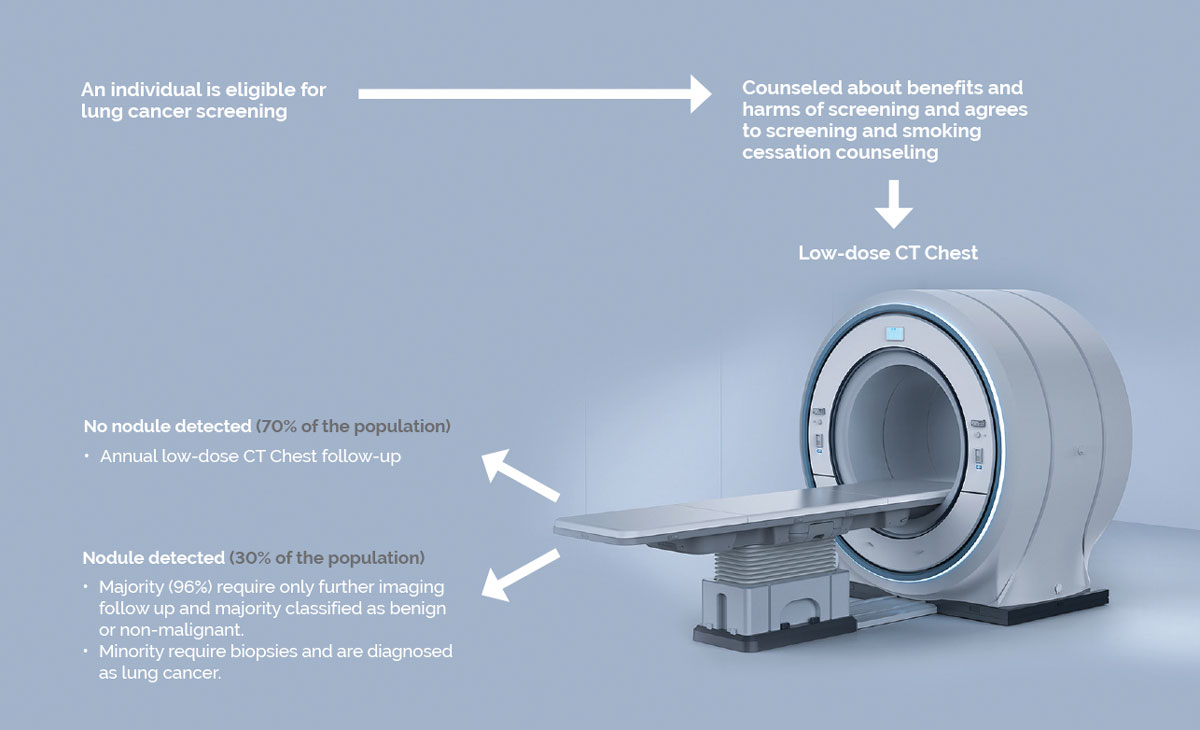
Lung cancer screening became standard of care after the results of the National Lung Cancer Screening Trial (NLST) conducted in the US between 2002 and 2009 were published. The trial compared low dose radiation computed tomography scans (LDCT) to chest X-rays in 53,456 participants (26,723 in the low-dose CT group and 26,733 in the radiography group). Based on the results of the NLST, the US Preventative Services Task Force recommended lung cancer screening with LDCT for those with the following risk factors:
- 55-80 years of age
- Current smokers or former smokers who quit less than 15 years ago
- Smokers of at least 30 pack-years (1 pack per day for 30 years or 2 packs per day for 15 years, etc…)
- In good health to undergo lung cancer surgery, which may involve removal of part of the lung (lobectomy) if needed. As people whose lungs are not fit for surgery were not part of the study, it has not been determined whether they would benefit from screening.
What are the benefits of lung cancer screening?
- Reducing death rate from lung cancer
- Without screening, the rate of death from lung cancer is 21 out of every 1,000 people vs 18 out of every 1,000 people with cancer screening.
- This means that with LDCT screening, 3 fewer people will die from lung cancer out of every 1,000 people.
- For every 320 people who are screened, 1 lung cancer death is prevented.
- Reducing death rate from any cause (not just lung cancer)
- In the absence of lung cancer screening, 75 out of every 1,000 people will die from any cause.
- If 1,000 people are screened once a year with LDCT for 3 years, 70 will die from any cause.
- This means that with LDCT screening, 5 fewer people will die from any cause.
Are there any harms to lung cancer screening?
- False alarms that lead to unnecessary additional testing
- Out of 1,000 people screened, 356 will have a false alarm.
- 18 of those will undergo invasive procedures for non-malignant disease (biopsies)
- 0.4 will have complications from procedure (bleeding, infection, collapsed lung, etc…)
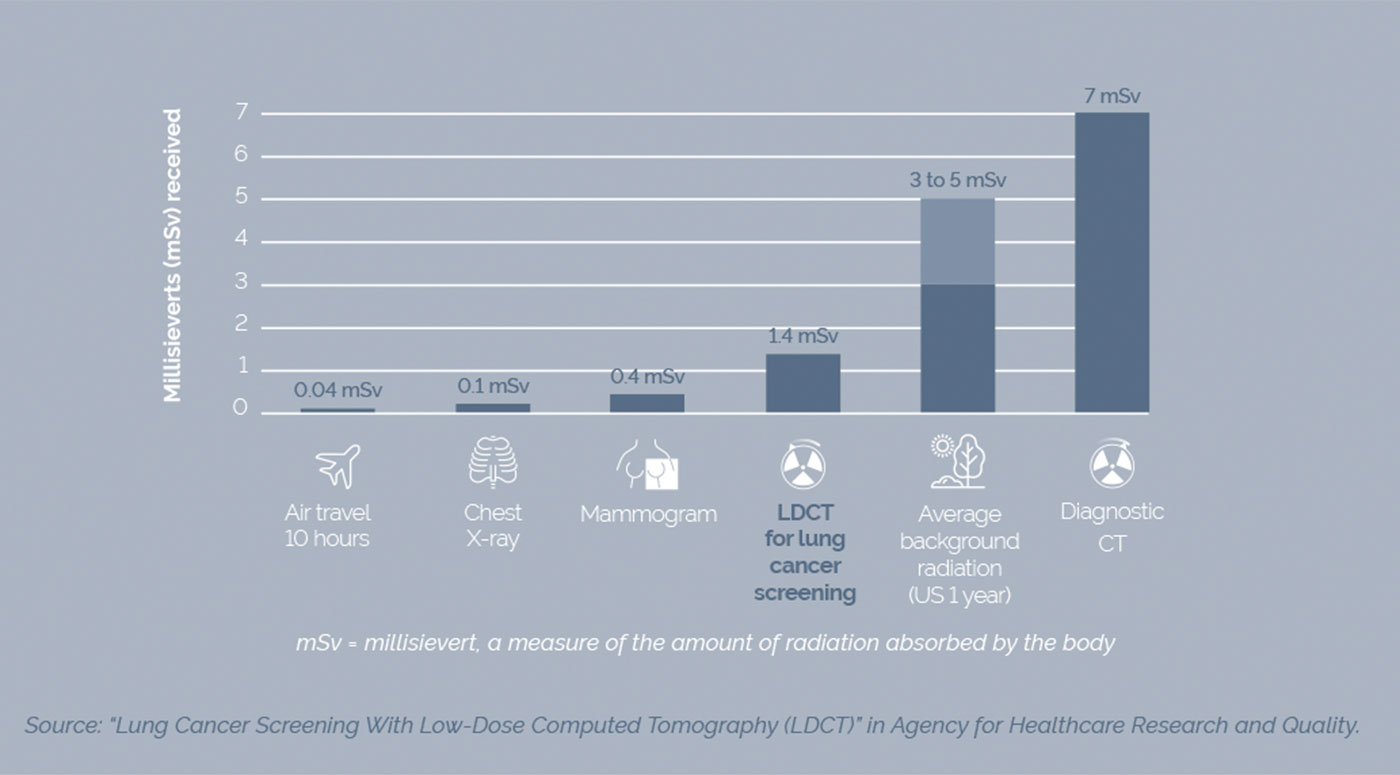
- Radiation exposure
- LDCT has a lower dose of radiation than a CT chest at 1.4 mSV. However, if there are positive findings on LDCT that require further follow-up, the patient will be exposed to much higher doses of radiation multiple times.
- Overdiagnosis
- Finding slow-growing lung cancers that may not have caused symptoms or harmed the patient
- Researchers found that for every 10 lung cancer cases detected via screening, one to two patients are treated for cancer that, in all likelihood, would not have harmed them.
- Findings outside the lungs
- On the CT scan, the radiologist could find other incidental issues such as an enlarged thyroid gland, or an enlarged aorta that need further investigation. It is not known whether detecting these early would affect one’s long-term health.
It is always important to discuss the benefits and risks of lung cancer screening with a physician before undergoing the first low dose radiation scan. Lung cancer screening is not an alternative to quitting smoking. Quitting smoking will decrease the risk of all cancers.
Electronic Cigarettes
What are electronic cigarettes?
They are cartridges of various types that contain nicotine and other substances – which may include formaldehyde – that create the reaction that leads to smoke in the cartridge.
Are electronic cigarettes as harmful as regular cigarettes?
Preliminary studies are showing that electronic cigarettes cause the same harm over the short term as regular cigarettes. They can lead to increased asthma symptoms, coughing, and wheezing or whistling sounds in the chest.
Because they are relatively new to the market, their long-term harm has not been adequately studied. Research to date indicates that they may pose the same risk of chronic obstructive pulmonary disease (COPD) as regular cigarettes, and that they are associated with a higher risk of cancers than for nonsmokers, although the risk may be lower than smoking regular cigarettes.
Should I try electronic cigarettes?
If you are not a smoker, you should not try them as they will lead to addiction and to potential harmful effects over the short and long term. If you are a smoker and want to quit, they may be a slightly safer alternative to smoking.
 Dr. Khalil Diab is clinical associate professor in the Department of Internal Medicine, Division of Pulmonary Diseases & Critical Care Medicine at the LAU Gilbert and Rose-Marie Chagoury School of Medicine. He specializes in interventional pulmonology with a focus on the diagnosis, staging, genomic analysis, and bronchoscopic treatment of lung cancer.
Dr. Khalil Diab is clinical associate professor in the Department of Internal Medicine, Division of Pulmonary Diseases & Critical Care Medicine at the LAU Gilbert and Rose-Marie Chagoury School of Medicine. He specializes in interventional pulmonology with a focus on the diagnosis, staging, genomic analysis, and bronchoscopic treatment of lung cancer.